You think you own your health data. You’re wrong.
Note: This article is for educational and informational purposes only. See full disclaimer at the end.
Imagine writing a journal about your health—every ache, every prescription, every diagnosis—but that journal is torn apart and scattered across dozens of locked cabinets, none of which you control.
Right now, as you read this, your medical information exists in dozens of different systems, owned by different companies, governed by different rules, and protected by different standards. Your blood test results live in one database. Your prescription history sits in another. Your fitness tracker data streams to a third. Your medical images are stored in a fourth. And you—the person this data is actually about—may have little to no control over any of it.
This isn’t just an academic concern. In 2024, healthcare suffered more cyberattacks than any other industry, with over 277 million patient records breached [1]—including the largest healthcare data breach in history when Change Healthcare was attacked, compromising the personal health information of 190 million Americans [2]. That’s more than half the U.S. population affected by a single breach.
But here’s what most people don’t realize: the same fragmentation that makes healthcare data vulnerable also makes it powerful when you take control of it. When you take control of that scattered data, you’re not just protecting yourself—you’re unlocking a powerful health optimization system.
Today, we’re going to change the dynamic. You’re going to understand exactly who owns your health data, where it lives, how to get it, and most importantly, how to control it.
A Common Story
Meet James, 42, recovering from long COVID. His pulmonologist couldn’t access his imaging from urgent care. His physical therapist had no idea about his prior autoimmune diagnosis. And James, stuck in a fog of fatigue, couldn’t remember which meds he was still taking. The data was out there—but scattered across five portals, three providers, and none of it fully in his hands. Sound familiar?
Whether it’s James, you, or someone you love, these stories happen every day around the world. Each one is a reminder: owning your health data isn’t about control for its own sake. It’s about survival, coherence, and peace of mind.
The Legal Reality: Access vs. Ownership
Let’s start with the uncomfortable truth: in most cases, you don’t legally own your health data. You have rights to access it, but ownership is a different matter entirely.
Under HIPAA (the Health Insurance Portability and Accountability Act), you have the right to access and obtain copies of your health information from covered entities—hospitals, doctors, health plans, and their business associates [3]. But HIPAA grants access rights, not ownership rights. The distinction matters more than you might think.
Only one U.S. state—New Hampshire—actually deems information in medical records to be the property of the patient [4]. Five states (Alaska, Colorado, Florida, Georgia, and Louisiana) grant patients ownership of their genetic information specifically [4]. Everywhere else? The legal framework is murky at best.
Meanwhile, in Europe, the General Data Protection Regulation (GDPR) takes a different approach [5]. While it doesn’t grant ownership per se, it provides much stronger individual rights over personal data, including health information. Europeans can access, correct, port, and even request deletion of their health data under certain circumstances [5]. The contrast with the U.S. system is stark.
But here’s the reality that transcends legal frameworks: whoever controls your health data controls your healthcare options. And right now, that’s probably not you.
The $34 Billion Health Data Economy
Your health data isn’t just sitting in medical records gathering digital dust. It’s feeding a massive industry. The global health data market is expected to reach $34.27 billion by 2025, growing at 22% annually [4].
Every click, every prescription, every test result, every doctor visit generates data that has commercial value.
Electronic Health Record companies, data analytics firms, pharmaceutical companies, insurance companies, and medical device manufacturers all profit from health data. Sometimes this benefits patients through better treatments and lower costs. But often, it simply enriches intermediaries while patients—the source of the data—see no benefit and maintain no control.

This isn’t necessarily malicious. Many uses of health data drive genuine medical breakthroughs. But the current system treats patients as passive data sources rather than active participants in the data economy. That’s what we’re going to change.
This massive economic value creates a troubling dynamic: the more valuable health data becomes, the bigger the target on healthcare organizations’ backs.
When billions of dollars flow through data pipelines, cybercriminals take notice. And unfortunately, the rush to capitalize on health data hasn’t been matched by equal investment in protecting it.
The Great Breach Crisis: Why This Matters Now
Healthcare data breaches aren’t just increasing—they’re exploding.
In 2024, the FBI reported that healthcare suffered more cyberthreats than any other critical infrastructure industry, with 444 reported incidents including 238 ransomware attacks and 206 data breaches [6].
The Change Healthcare attack in February 2024 disrupted healthcare operations nationwide and exposed the personal health information of 190 million people [2]. But it wasn’t an isolated incident.
Major breaches hit Kaiser Foundation Health Plan (13.4 million affected), Ascension Health (437,000 affected), and dozens of other healthcare organizations [2].
Why are healthcare organizations such attractive targets? Because health data is incredibly valuable on the black market. A complete medical record can sell for $250-$1,000 on the dark web—10 to 40 times more than a credit card number [7].
Health data includes everything identity thieves need: Social Security numbers, dates of birth, addresses, insurance information, and detailed personal histories that never change.
But here’s the crucial point:
When your data is scattered across dozens of systems with varying security standards, you’re only as protected as the weakest link.
Centralized control of your health data—with you as the controller—isn’t just about convenience. It’s about security.

Understanding Your Data Ecosystem
Every data type—clinical, digital, genetic, or behavioral—lives in its own system, bound by its own rules. To control your health, you need to map that landscape.
Your health information exists in several distinct categories:
Electronic Health Records (EHRs)
These are the comprehensive digital records maintained by healthcare providers. They include your medical history, medications, lab results, radiology reports, and clinical notes. EHRs are designed primarily for provider use, though patients have access rights under HIPAA.
Personal Health Records (PHRs)
These are patient-controlled digital records where you can store and manage your own health information. Some are offered by healthcare providers (like patient portals), others are standalone platforms that aggregate data from multiple sources.
Device and App Data
Your fitness tracker, smartphone health apps, home monitoring devices, and wearable technology generate continuous streams of health-related data. This information often lives in consumer platforms with different privacy rules than traditional healthcare data.
Genomic and Laboratory Data
Genetic testing results, lab work, and specialized testing often live in separate systems managed by testing companies, laboratories, or specialized genomic data companies.
Insurance and Claims Data
Your health insurance company maintains detailed records of your medical history based on claims, pre-authorizations, and coverage decisions. This data can be extensive and includes information from multiple providers.
Pharmacy Records
Prescription history, medication adherence data, and drug interaction information typically live in pharmacy benefit management systems and retail pharmacy platforms.
Each category operates under different rules, with different access procedures, different security standards, and different sharing protocols. The fragmentation isn’t accidental—it’s often profitable for intermediaries and convenient for providers. But it’s terrible for patients.
The FHIR Revolution: Making Data Move
Thankfully, the healthcare industry is slowly beginning to address this fragmentation—and the most promising development so far is FHIR.
FHIR (Fast Healthcare Interoperability Resources) is reshaping how health systems talk to each other—securely, flexibly, and in real time. It’s a standard that enables health information systems to communicate using modern web technologies [8].

FHIR breaks health data into modular ‘resources’—like puzzle pieces that can be shared individually across systems [8]. This replaces the old model of all-or-nothing record access with granular, patient-directed control. Need to share just your medication list with a new doctor? FHIR makes that possible without exposing your entire medical history [8].
The 21st Century Cures Act, fully implemented in 2022, requires healthcare providers to give patients unfettered digital access to their health information using standards like FHIR [9]. This means you can now request your complete health records in digital format without paying fees for printed copies or waiting weeks for fax transmissions.
Building Your Health Data Sovereignty Framework
Taking control of your health data requires a systematic approach. I call it the Health Data Sovereignty Framework—a practical protocol for mapping, accessing, controlling, and protecting your health information.
Phase 1: Assessment (Week 1)
Start by mapping your current health data landscape. Create a comprehensive inventory:
Provider Inventory:
- Primary care physicians (current and past 5 years)
- Specialists you’ve seen
- Hospitals where you’ve received care
- Urgent care and emergency room visits
- Laboratory companies (Quest, LabCorp, hospital labs)
- Imaging centers
- Pharmacies (retail and specialty)
Digital Platform Inventory:
- Patient portals you have access to
- Health apps on your phone
- Wearable devices and fitness trackers
- Health-related online accounts
- Insurance member portals
Data Type Inventory:
- Laboratory results and trends
- Imaging studies (X-rays, MRIs, CT scans)
- Prescription history
- Immunization records
- Surgical and procedure reports
- Clinical notes and visit summaries
- Genetic testing results
- Device-generated data (blood pressure, glucose, heart rate)
This inventory becomes your roadmap for data recovery and organization. Go far as back as you can, the more you can gather, the better.
Phase 2: Access (Weeks 2-4)
Now begins the systematic process of requesting and collecting your health data. Under HIPAA, covered entities must provide your health information within 30 days of a written request, though many can respond much faster.
Digital-First Strategy: Most healthcare organizations now offer patient portals or digital access platforms. Start here because digital records are easier to organize and share than paper copies.
Comprehensive Requests: Don’t just request “medical records.” Be specific [3]:
- “Complete medical record including all clinical notes, lab results, imaging studies, and communications about my care”
- “All data in your designated record set related to my care”
- “Electronic copies in the most accessible format available”
Leverage the 21st Century Cures Act: Healthcare providers cannot charge you for electronic copies of your health information, and they cannot require you to use their specific patient portal if you want to send your data elsewhere.
Document Everything: Keep records of all data requests, including dates, contact information, and any fees charged. If providers are non-responsive or charge excessive fees, you can file complaints with the Office for Civil Rights.
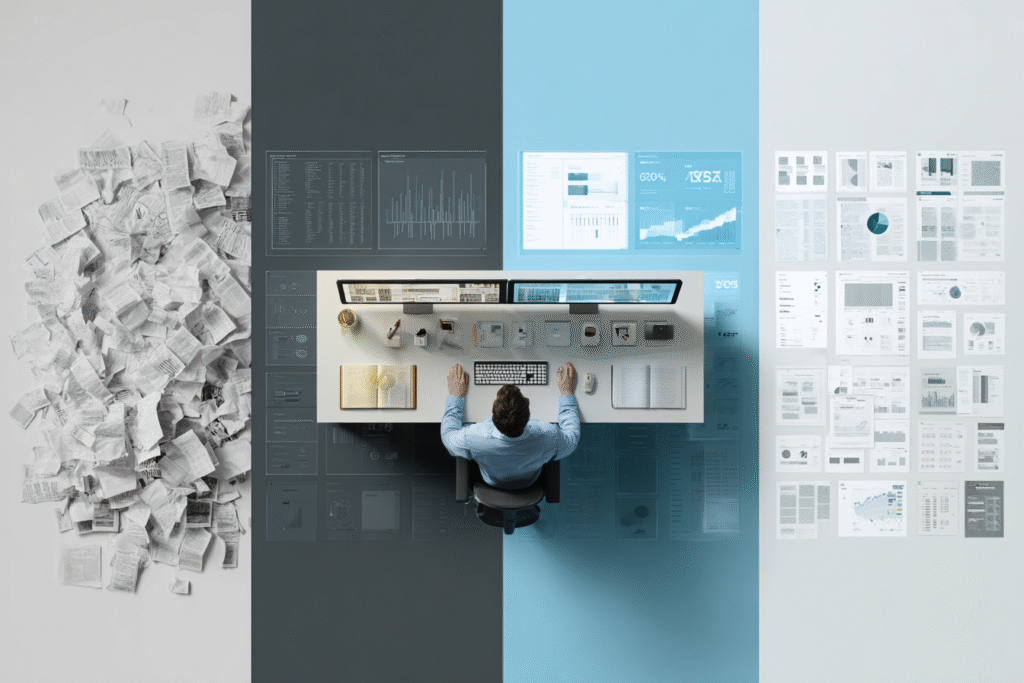
Phase 3: Control (Weeks 5-6)
Once you’re collecting your health data, you need systems for organization, storage, and access control.
Choose Your Platform Strategy: You have several options for consolidating your health data:
Personal Health Record (PHR) Platforms: Services like Apple Health Records, or Epic MyChart can aggregate data from multiple sources.
Cloud Storage: Secure cloud storage with healthcare-grade encryption provides complete control but requires more technical management.
Hybrid Approach: Use PHR platforms for active data and secure storage for comprehensive archives.
Implement Access Controls:
- Use strong, unique passwords for all health-related accounts
- Enable two-factor authentication wherever possible
- Regularly review who has access to your data
- Understand sharing permissions and how to revoke them
Standardize Data Formats: When possible, request data in FHIR-compatible formats. This makes it easier to move data between systems and enables better integration with health apps and AI tools.
Phase 4: Protection (Ongoing)
Health data security requires constant vigilance, especially as cyber threats targeting healthcare continue to escalate.
Security Best Practices:
- Use healthcare-grade encryption for stored data
- Regularly update software and security settings
- Monitor accounts for suspicious activity
- Use secure networks (not public WiFi) for health data access
- Back up critical health information in multiple locations
Sharing Protocols: Develop clear criteria for when and how you’ll share health data:
- Only share with verified healthcare providers
- Understand what data sharing permissions you’re granting
- Read privacy policies before connecting to new platforms
- Use time-limited sharing when possible
- Document who has access to what information
Breach Response Plan: Know what to do if your health data is compromised:
- Monitor credit reports and healthcare benefit statements
- Contact your healthcare providers about potential fraud
- File complaints with appropriate authorities
- Change passwords and access credentials
- Consider credit freezes and fraud alerts
Now that your systems are secure, let’s look at the tools that can support you along the way.
Practical Tools and Platforms
The health data management landscape is evolving rapidly. Here are the most effective tools and platforms currently available:
Personal Health Record Platforms
Apple Health Records: Integrates with many healthcare systems and aggregates data from multiple sources. Strong privacy protections and user control. Works seamlessly with Apple devices and health apps [10].
Epic MyChart: Many healthcare systems use Epic EHRs, and MyChart provides comprehensive access to your data within those systems. Can share data with other Epic-connected systems [10].
Google Health: Google’s health data platform with AI-powered insights. Integration with Fitbit and other Google services. Consider privacy implications of Google’s broader data practices.
Data Aggregation Services
Hugo Health: Helps patients collect and organize health data from multiple sources. Focused on patient control and data portability, they can seamlessly link your health information to research studies.
Picnic Health: Creates comprehensive health records by collecting data from all your providers. Useful for patients with complex medical histories or multiple providers.
Citizen: Rare disease-focused platform that aggregates medical records and makes them available for research. Good example of patient-controlled data sharing for medical advancement.
Security and Storage Solutions
Healthcare-Grade Cloud Storage: Services like Box, Dropbox Business, or Amazon Web Services that offer HIPAA-compliant storage options.
Encrypted Health Apps: Apps like HealthTap or Amwell that provide secure communication with healthcare providers.
Password Management: Use dedicated password managers for health accounts to ensure strong, unique passwords.
Safe Data Sharing: Evaluation Framework
As you take control of your health data, you’ll face decisions about sharing it with new platforms, apps, and services. Not all data sharing is created equal.

Here’s a framework for evaluation:
Green Light Criteria
- Clear, specific privacy policies
- Healthcare industry compliance (HIPAA, HITECH)
- Strong encryption and security measures
- User control over data sharing and deletion
- Transparent business model (how they make money)
- Positive track record with data security
- Easy data export options
Examples: Apple Health Records (clear data portability), Epic MyChart (established healthcare compliance), Hugo Health (transparent patient-control focus)
Yellow Light Criteria
- Broad or vague privacy policies
- Limited user control over data sharing
- Business model based on advertising or data sales
- Recent changes in ownership or privacy policies
- Limited security track record
Examples: Newer fitness apps with broad data requests, platforms recently acquired by larger companies, services offering “free” health insights without clear revenue models
Red Light Criteria
- Unclear or absent privacy policies
- No healthcare compliance measures
- History of data breaches or security issues
- Business model requires selling user data
- Difficult or impossible data deletion
- Requests for unnecessary permissions
- Pressure tactics or time-limited offers
Examples: Apps requesting location data for basic health tracking, platforms without visible privacy policies, services that won’t allow data deletion or export
Special Considerations for Family Data: If you manage health data for family members, especially children or elderly relatives, apply even stricter criteria. Their data may be more vulnerable and have longer-term implications.
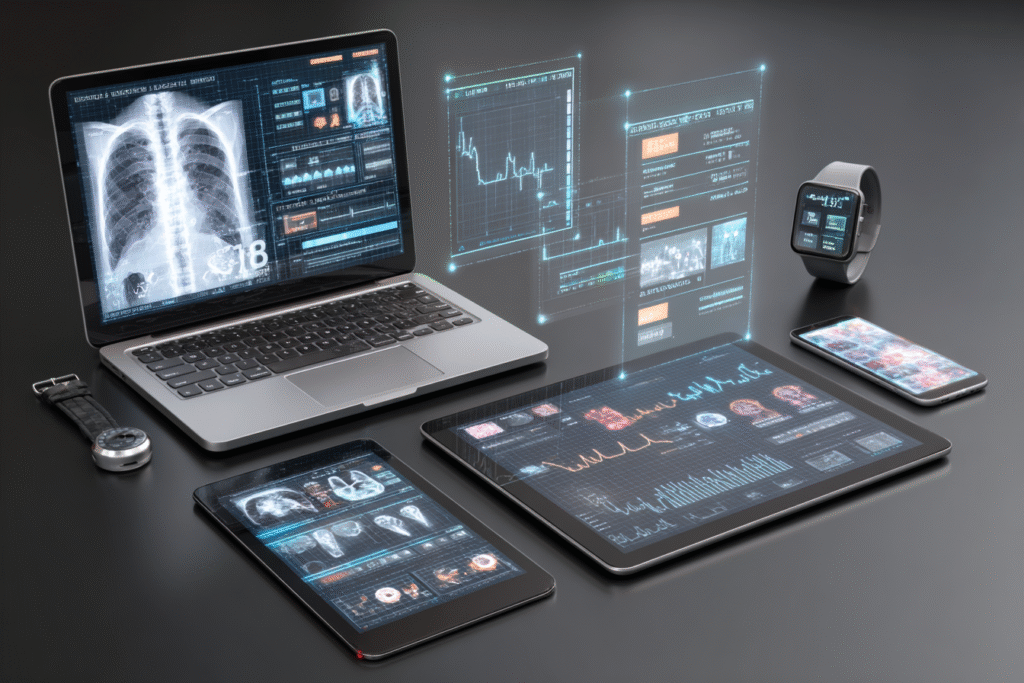
The AI-Health Data Connection
Everything we’ve covered today connects directly to the AI-driven health revolution we’ve been exploring in this series.
Remember the AI Partnership Protocol from Day 50? The four phases—Signal Integration, Pattern Recognition, Predictive Intervention, and Adaptive Learning—all depend on comprehensive, high-quality health data.
But here’s the crucial insight:
AI’s effectiveness is directly proportional to data quality and completeness.
Fragmented data produces fragmented insights. Incomplete data leads to missed patterns. Inconsistent data formats limit AI’s ability to provide personalized recommendations.

When you take control of your health data and consolidate it into comprehensive, well-organized records, you’re not just exercising your rights as a patient. You’re building the foundation for AI-enhanced health optimization.
You can’t effectively monitor what you can’t measure, and you can’t measure what you don’t control.
Building Toward Proactive Health Ownership
The Health Data Sovereignty Framework isn’t just about organizing what you have—it’s about building toward what’s possible. When you control your health data comprehensively, several transformative capabilities emerge:
Longitudinal Pattern Recognition: You can identify health trends and patterns that span multiple providers and time periods. This is impossible when your data is fragmented across different systems.
Informed Decision Making: Complete health data enables better healthcare decisions. You can see the full context of your health journey, identify what treatments have worked, and make more informed choices about future care.
Research Participation: With control over your comprehensive health data, you can choose to participate in research studies that might benefit your specific condition or contribute to medical knowledge.
AI-Enhanced Health Optimization: Comprehensive, well-organized health data is the foundation for the AI health applications we’ve been exploring. The more complete your data, the better AI can help optimize your health.
Emergency Preparedness: In medical emergencies, having immediate access to your complete health information can be life-saving. Emergency responders, new physicians, and specialists can quickly understand your medical history, current medications, and potential complications.
Family Health Legacy: By organizing and maintaining your health data, you create a valuable resource for family members who may share genetic risk factors or health concerns.
Implementation Checklist
Now it’s time to move from clarity to action.
This checklist isn’t just a to-do list — it’s a blueprint for sovereignty. Over the next six weeks, you’ll build a personal health data system that gives you visibility, control, and security.
Whether you’re just starting or filling in the gaps, each step compounds your ability to optimize your health with intention and intelligence.
Week 1: Assessment (2-3 hours total)
- Create provider inventory (last 5 years) [45 minutes]
- List all digital health platforms and apps [30 minutes]
- Inventory all types of health data you’ve generated [45 minutes]
- Identify gaps in your current data access [30 minutes]
Week 2: Initial Access Requests (3-4 hours total)
- Request records from primary care physician [30 minutes]
- Request records from most recent specialists [60 minutes]
- Download data from patient portals [90 minutes]
- Request laboratory results from past 2 years [45 minutes]
Week 3: Comprehensive Data Collection (4-5 hours total)
- Request imaging studies and reports [60 minutes]
- Collect prescription history from pharmacies [60 minutes]
- Gather insurance claims data [90 minutes]
- Export data from health apps and devices [60 minutes]
Week 4: Organization and Storage Setup (3-4 hours total)
- Choose your data management platform [60 minutes research]
- Set up secure storage with appropriate encryption [90 minutes]
- Organize data by type and date [90 minutes]
- Create backup copies in secondary location [45 minutes]
Week 5: Access Control Implementation (2-3 hours total)
- Update passwords for all health-related accounts [60 minutes]
- Enable two-factor authentication [45 minutes]
- Review and adjust privacy settings [45 minutes]
- Document sharing permissions [30 minutes]
Week 6: Security and Sharing Protocols (2-3 hours total)
- Implement ongoing security monitoring [45 minutes setup]
- Create data sharing evaluation criteria [30 minutes]
- Establish emergency access procedures [45 minutes]
- Document your data management decisions [30 minutes]
Ongoing Maintenance:
- Monthly: Review account security and access logs
- Quarterly: Update your health data inventory
- Annually: Comprehensive security review and system updates
By this point, you’ve moved from scattered awareness to structured sovereignty. You’ve built a system—not just of data collection, but of control. And it’s from this foundation that everything else becomes possible.
The Road Ahead
Taking control of your health data is more than an administrative exercise—it’s a fundamental shift toward health empowerment. You’re moving from being a passive recipient of healthcare to an active participant in your health optimization.
This foundation supports everything we’ve built in this series so far: the Reality Architecture framework that helps you see clearly, the SIMPLE decision-making process that helps you act effectively, and the AI Partnership Protocol that helps you leverage technology intelligently.
Your health data is the story of your body’s journey through time.
For too long, that story has been scattered across different systems, controlled by different entities, and written in languages you couldn’t read. Today, you’ve learned how to reclaim authorship of your own story.
Having control over your data is just the beginning—knowing how to use it wisely is what transforms information into health transformation.
The revolution in healthcare isn’t coming—it’s here. And it starts with you taking control of your own health information.
Your data. Your decisions. Your health. Your life.
See you in the next insight.
Comprehensive Medical Disclaimer: The insights, frameworks, and recommendations shared in this article are for educational and informational purposes only. They represent a synthesis of research, technology applications, and personal optimization strategies, not medical advice. Individual health needs vary significantly, and what works for one person may not be appropriate for another. Always consult with qualified healthcare professionals before making any significant changes to your lifestyle, nutrition, exercise routine, supplement regimen, or medical treatments. This content does not replace professional medical diagnosis, treatment, or care. If you have specific health concerns or conditions, seek guidance from licensed healthcare practitioners familiar with your individual circumstances.
References
- The HIPAA Journal. “Healthcare Data Breach Statistics.” HIPAA Journal, May 26, 2025. https://www.hipaajournal.com/healthcare-data-breach-statistics/
- McKeon, Jill. “10 largest healthcare data breaches of 2024.” TechTarget, 2024. https://www.techtarget.com/healthtechsecurity/feature/Largest-healthcare-data-breaches
- U.S. Department of Health and Human Services. “Individuals’ Right under HIPAA to Access their Health Information.” HHS.gov, January 5, 2016. https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/access/index.html
- Price, W. Nicholson, and I. Glenn Cohen. “Patient data ownership: who owns your health?” PMC, 2021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8487665/
- GDPR.eu. “What is GDPR, the EU’s new data protection law?” GDPR.eu, August 29, 2024. https://gdpr.eu/what-is-gdpr/
- American Hospital Association. “Report: Health care had most reported cyberthreats in 2024.” AHA News, May 12, 2025. https://www.aha.org/news/headline/2025-05-12-report-health-care-had-most-reported-cyberthreats-2024
- SecureFrame. “110+ of the Latest Data Breach Statistics [Updated 2025].” SecureFrame, January 3, 2025. https://secureframe.com/blog/data-breach-statistics
- HealthIT.gov. “Health Level 7 (HL7) Fast Healthcare Interoperability Resources (FHIR).” HealthIT.gov. https://www.healthit.gov/topic/standards-technology/standards/fhir
- Ross, Casey. “Call it data liberation day: Patients can now access all their health records digitally.” STAT News, October 6, 2022. https://www.statnews.com/2022/10/06/health-data-information-blocking-records/
- InformationWeek. “9 Popular Personal Health Record Tools.” InformationWeek. https://www.informationweek.com/machine-learning-ai/9-popular-personal-health-record-tools