What if the most complex health mysteries have embarrassingly simple answers we’re too sophisticated to see?
Note: This article is for educational and informational purposes only. See full disclaimer at the end.
Alita had seen twelve specialists in three years. Her chart was a collage of labels: chronic fatigue, migrating joint pain, brain fog thick enough to miss her daughter’s recital, and a gut so temperamental she mapped bathrooms within a five-mile radius. Each new consult added a diagnosis, a medication, and another layer of complexity.
Specialist thirteen — a systems-minded clinician — opened with a question no one had asked:
“How much water do you drink?”
Alita laughed. Then cried. Most days: two coffees, a diet soda, a glass of wine. Actual water? Almost none.
Six weeks later, after consistent hydration (with electrolytes), she called again — this time crying with relief.
For Alita, the fog lifted. Energy improved. Joint pain significantly decreased. Three years, twelve specialists, thousands of dollars — and the first big lever appeared to be hydration.
The Sophistication Trap
We live in an age where you can order a genome report with your groceries. It conditions us to expect complex solutions to complex problems. When symptoms span multiple systems, we leap to exotic explanations — autoimmune cascades, rare genetics, mystery syndromes.
Yet complex bodies often fail in simple, predictable ways. Like a high-end computer crashing because it wasn’t plugged in, basic deficits can produce Byzantine symptom maps: low intake, low sun, low sleep, low movement, high stress.
Two common contributors sometimes mistaken for “mystery illness”: inadequate hydration and low vitamin D. Both influence cognition, mood, immunity, and endocrine tone — and both are easy to miss when the system incentivizes categorizing symptoms instead of stabilizing the system [1] [2] [3] [5] [6] [16].
If you’re thinking ‘it can’t be that simple’—you’re right. And wrong. Simple doesn’t mean easy, and foundational doesn’t mean superficial.
The basics require consistency, humility, and patience.
They work slowly, quietly, without the drama of a breakthrough. That’s precisely why we overlook them.
The Pattern Recognition Problem
A systems view asks, “What single upstream change could harmonize these downstream complaints?”
Consider thyroid dysfunction. Its symptoms sprawl: fatigue, weight gain, depression, hair loss, constipation, brain fog, cold intolerance. Thyroid disorders are common in the U.S. [17].
Compounding the trap: the thyroid issue may itself be secondary. Low vitamin D status is associated with autoimmune thyroid disease; immune dysregulation upstream can look like “thyroid disease” downstream [5] [6].
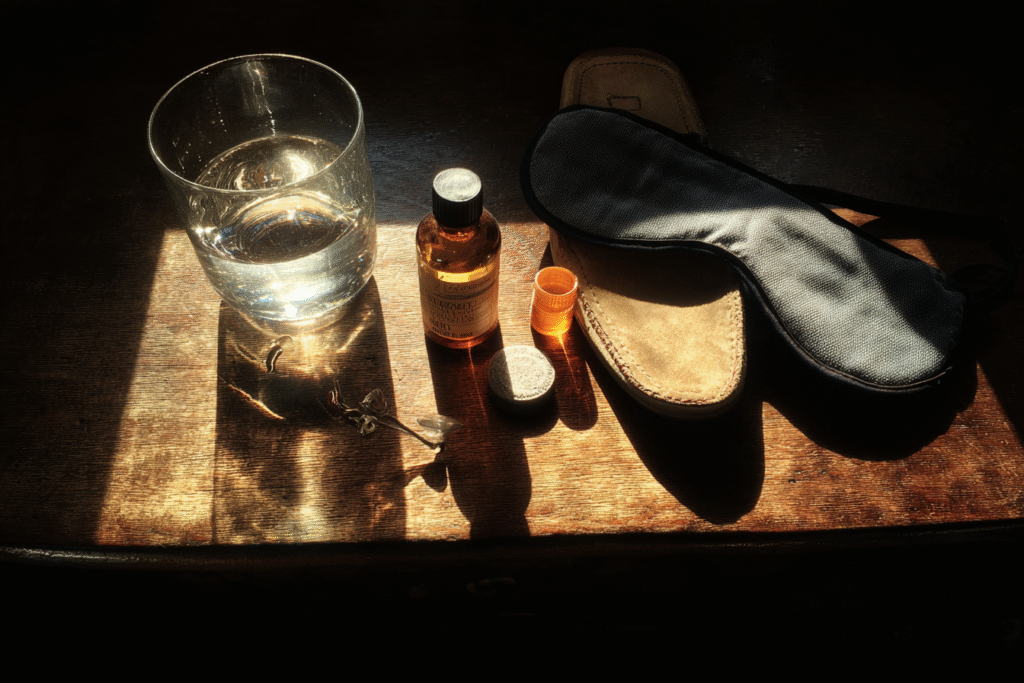
Water: The Missing First Step
Even mild dehydration can impair attention, working memory, reaction time, and mood; rehydration can improve some effects within hours [1][2][3].
Longer-term data link poorer hydration with faster cognitive decline in older adults [4].
14-day baseline move
• Target ~0.5–0.7 oz per lb of body weight daily (adjust for heat/activity).
• Add electrolytes if you sweat, train, sauna, or rely on diuretics.
• Front-load earlier in the day; finish 2–3 hours before bed.
Track mood, focus, stool quality, energy, and pain daily.

Vitamin D: Small Molecule, Big Edges
Vitamin D receptors are widespread across immune, endocrine, and neural tissues. Low levels are associated in research with higher autoimmune risk (including autoimmune thyroiditis) and with inflammatory and mood disturbances [5] [6].
Testing and optimal levels remain debated—work with your clinician to determine if you need testing based on your risk factors and symptoms. Most experts agree that documented deficiency should be corrected, but routine screening of healthy adults remains controversial [14] [16] [20] [21].
The Gut You’re Relying On
You can’t supplement your way past malabsorption. Processed diets, stress, antibiotics, and low stomach acid can blunt uptake — especially for fat-soluble vitamins like D.
The gut harbors a large share of the body’s immune cells, and gut–immune cross-talk shapes systemic inflammation [9] [10].
The gut influences mood and cognition through immune and inflammatory pathways—not by sending serotonin directly to your brain as commonly claimed. When your gut is inflamed, your whole system feels it [11] [12] [13].
And when your gut is struggling—bloated, inflamed, or simply working overtime to process a late dinner—quality sleep becomes nearly impossible.
Sleep: The Silent Multiplier
Sleep is when your body performs repair, memory consolidation, glymphatic clearance, immune recalibration, and hormone synchronization.
Short sleep is associated with elevated inflammatory signaling and higher cardiometabolic risk; most adults should aim for ≥7 hours regularly [7] [8].
14-day baseline move
• Fixed sleep/wake window (±30 min), cool/dark/quiet room, dim lights after sunset, caffeine cutoff ≥8 h before bed, park the phone outside the room.
Movement: Consistency Beats Intensity
Stress: The Amplifier
Chronic stress impairs nutrient absorption, fragments sleep, ramps inflammation, and dysregulates immune signaling — turning simple problems into complex syndromes.
The marketing director who thought she had chronic fatigue syndrome discovered her symptoms lifted when she stopped checking email after 8pm. The teacher whose ‘fibromyalgia’ improved dramatically after setting boundaries with demanding parents.
Meta-analytic evidence shows sustained stress suppresses multiple immune parameters [15].
Daily downshift (10–20 min)
• One of: breathwork, prayer, nature walk, journaling, guided relaxation, honest boundaries.
• Track perceived stress (0–10) and morning resting heart rate.
The Troubleshooting Framework (Do This First)
Water first. Two weeks, consistent hydration; add electrolytes if needed [1] [2] [3] [4].
Vitamin D. Discuss testing/targets with your clinician; correct documented low status and re-check [14] [16] [20].
Stabilize the gut. Aim for symptom-free digestion before stacking protocols [9] [10] [11] [12].
Audit sleep. Standardize timing; guard darkness and temperature [7] [8].
Move gently, daily. Walks, mobility, basic strength — earn intensity [18] [19].
Diffuse stress. One intentional downshift practice every day [15].
Consider running this 14-day baseline to inform next steps before adding labs or supplements (unless red flags are present). If red flags appear (chest pain, neuro deficits, GI bleeding, rapid weight loss, persistent fever, severe depression), escalate care immediately.
RED FLAGS: When Simple Isn't Enough
Simple solutions apply to chronic patterns, not acute crises. Seek immediate medical attention for:
- Chest pain or pressure
- Sudden neurological changes (weakness, numbness, vision loss, severe headache)
- GI bleeding (black stools, blood in vomit)
- Unexplained rapid weight loss (>5% in a month)
- Persistent fever without clear cause
- Severe depression or thoughts of self-harm
These symptoms deserve urgent evaluation—don’t delay care trying water first.
The Implementation Reality
The paradox: simple is harder than complicated because it demands consistency. Healthcare excels at acute rescue; it struggles with daily scaffolding. That’s why ownership matters: water, sun, food, sleep, movement, boundaries — these live where you live.
The Stories We Rarely Share
The executive who reversed prediabetes with 30-minute walks and a sleep curfew. The mother whose migraines faded after restoring vitamin D. The student whose “depression” eased when nights became nights again.
These case studies illustrate what’s possible when foundations improve.
The Cost We Don't Calculate
The average American spends $13,000 annually on healthcare. The average specialist visit costs $400 and takes three weeks to schedule. A comprehensive metabolic panel runs $200-500. An MRI? $1,000-3,000.
A water bottle costs $20. Vitamin D supplements, $15 monthly. Better sleep hygiene, free. Daily walks, free. Saying no to commitments that drain you, priceless.
We’ve built a system that profits from complexity while the solutions that could prevent 80% of chronic disease cost less than a single specialist copay.
The question isn’t whether you can afford to prioritize basics—it’s whether you can afford not to.

The Path Forward
Before you chase complexity, stabilize the basics to clarify the picture.
Give basic inputs a fair runway (4–6 weeks), and document everything — water, sleep, movement, symptoms, stress.
You’re not “guessing”; you’re running a structured experiment on the system you inhabit.
Your body isn’t broken. The system may be noisy, but your biology still remembers how to heal — especially when you give it the raw materials.
Sometimes the most advanced troubleshooting is checking whether it’s plugged in.
Alita still sees doctors regularly. But now she brings a water bottle to appointments.
See you in the next insight.
Comprehensive Medical Disclaimer: The insights, frameworks, and recommendations shared in this article are for educational and informational purposes only. They represent a synthesis of research, technology applications, and personal optimization strategies, not medical advice. Individual health needs vary significantly, and what works for one person may not be appropriate for another. Always consult with qualified healthcare professionals before making any significant changes to your lifestyle, nutrition, exercise routine, supplement regimen, or medical treatments. This content does not replace professional medical diagnosis, treatment, or care. If you have specific health concerns or conditions, seek guidance from licensed healthcare practitioners familiar with your individual circumstances.
References
The references below are organized by study type. Peer-reviewed research provides the primary evidence base, while systematic reviews synthesize findings.
Peer-Reviewed / Academic Sources
[1] Zhang, N., et al. (2019). Effects of dehydration and rehydration on cognitive performance and mood among male college students. International Journal of Environmental Research and Public Health, 16(11), 1891. https://pmc.ncbi.nlm.nih.gov/articles/PMC6603652/
[2] Ganio, M. S., et al. (2011). Mild dehydration impairs cognitive performance and mood of men. British Journal of Nutrition, 106(10), 1535–1543. https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/mild-dehydration-impairs-cognitive-performance-and-mood-of-men/3388AB36B8DF73E844C9AD19271A75BF
[3] Armstrong, L. E., et al. (2012). Mild dehydration affects mood in healthy young women. Journal of Nutrition, 142(2), 382–388. https://pubmed.ncbi.nlm.nih.gov/22190027/
[4] Nishi, S. K., et al. (2023). Hydration status and two-year cognitive change in older adults. BMC Medicine, 21, 314. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-023-02771-4
[5] Leko, M. B., Jureško, I., Rozić, I., Pleić, N., Gunjača, I., & Zemunik, T. (2023). Vitamin D and the thyroid: A critical review of the current evidence. International Journal of Molecular Sciences, 24(4), 3586. https://pmc.ncbi.nlm.nih.gov/articles/PMC9964959/
[6] Durá-Travé, T., Gallinas-Villarrubia, P., & Aguilera-Albesa, S. (2024). Autoimmune thyroiditis and vitamin D. International Journal of Molecular Sciences, 25(6), 3154. https://www.mdpi.com/1422-0067/25/6/3154
[7] Irwin, M. R. (2019). Sleep and inflammation: Partners in sickness and in health. Nature Reviews Immunology, 19, 702–715. https://www.nature.com/articles/s41577-019-0190-z
[8] Watson, N. F., et al. (2015). Recommended amount of sleep for a healthy adult (AASM/SRS consensus). Sleep, 38(6), 843–844. https://pmc.ncbi.nlm.nih.gov/articles/PMC4434546/
[9] Wiertsema, S. P., et al. (2021). The interplay between the gut microbiome and immune system. Frontiers in Immunology, 12, 1–15. https://pmc.ncbi.nlm.nih.gov/articles/PMC8001875/
[10] Belkaid, Y., & Harrison, O. J. (2017). Homeostatic immunity and the microbiota. Immunity, 46(4), 562–576. https://pubmed.ncbi.nlm.nih.gov/28423337/
[11] Bellono, N. W., et al. (2017). Enterochromaffin cells couple gut stimuli to serotonin release. Cell, 170(1), 185–198. https://pubmed.ncbi.nlm.nih.gov/28648659/
[12] Kanova, M., & Kohout, P. (2021). Serotonin—Its synthesis and roles in the healthy and the critically ill. International Journal of Molecular Sciences, 22(9), 4837. https://pmc.ncbi.nlm.nih.gov/articles/PMC8124334/
[13] El-Merahbi, R., Löffler, M., Mayer, A., & Sumara, G. (2015). The roles of peripheral serotonin in metabolic homeostasis. FEBS Letters, 589(15), 1728–1734. https://pubmed.ncbi.nlm.nih.gov/26070423/
[14] Demay, M. B., et al. (2024). Vitamin D for the prevention of disease (Endocrine Society clinical practice guideline). Journal of Clinical Endocrinology & Metabolism, 109(8), 1907–1932. https://academic.oup.com/jcem/article-abstract/109/8/1907/7685305
[15] Segerstrom, S. C., & Miller, G. E. (2004). Psychological stress and the human immune system: A meta-analytic study. Psychological Bulletin, 130(4), 601–630. https://pmc.ncbi.nlm.nih.gov/articles/PMC1361287/
Government / Institutional Sources
[16] National Institutes of Health — Office of Dietary Supplements (2025). Vitamin D: Health Professional Fact Sheet. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
[17] American Thyroid Association (n.d.). General Information / Press Room — Facts & Statistics. https://www.thyroid.org/media-main/press-room/
[18] Centers for Disease Control and Prevention (2023). Adult Physical Activity Guidelines. https://www.cdc.gov/physical-activity-basics/guidelines/adults.html
[19] Centers for Disease Control and Prevention (2024). Benefits of Physical Activity. https://www.cdc.gov/physical-activity-basics/benefits/index.html
[20] Endocrine Society (2024). Clinical Practice Guideline Hub — Vitamin D for the Prevention of Disease. https://www.endocrine.org/clinical-practice-guidelines/vitamin-d-for-prevention-of-disease
[21] Endocrine Society (2024). News Release — Healthy adults under 75: RDA is sufficient; routine testing not needed. https://www.endocrine.org/news-and-advocacy/news-room/2024/endocrine-society-recommends-healthy-adults-take-the-recommended-daily-allowance-of-vitamin-d